Cedars-Sinai's First Minimally Invasive Double Lung Transplant
Date
November 19, 2021

Date
November 19, 2021
Credits
Medical providers featured in this article
In Brief
{{cta-block}}
Last September, Frank Coburn took what he thought would be the last motorcycle ride of his life. Six months prior, at age 57, the previously active biker and boat mechanic was diagnosed with pulmonary fibrosis after years of declining health. Following the diagnosis, his local pulmonologist referred Coburn to the leading pulmonary fibrosis center at the Cedars-Sinai Women’s Guild Lung Institute, ranked #3 in the nation for pulmonology and lung surgery.
His care team ultimately recommended a bilateral lung transplant. In December 2020, already on the transplant list, Coburn tested positive for COVID-19. He rapidly declined and relied on full-time supplemental oxygen. Once he reached end-stage lung failure, Coburn advanced to the top of the list. While Coburn was eager for a transplant, he dreaded the significant scarring and lengthy recovery process. “I was concerned about the scar,” he said. “I ride shirtless often.”
Coburn was the first patient to undergo a minimally invasive double lung transplant at Cedars-Sinai, and likely the first in the United States.
"The bottom line is that recovery from minimally invasive lung transplant takes days rather than weeks. Reducing recovery time produces additional benefits for patients: shorter hospital stays, reduced risk for post-op infection and reduced need for medication, including opioids."
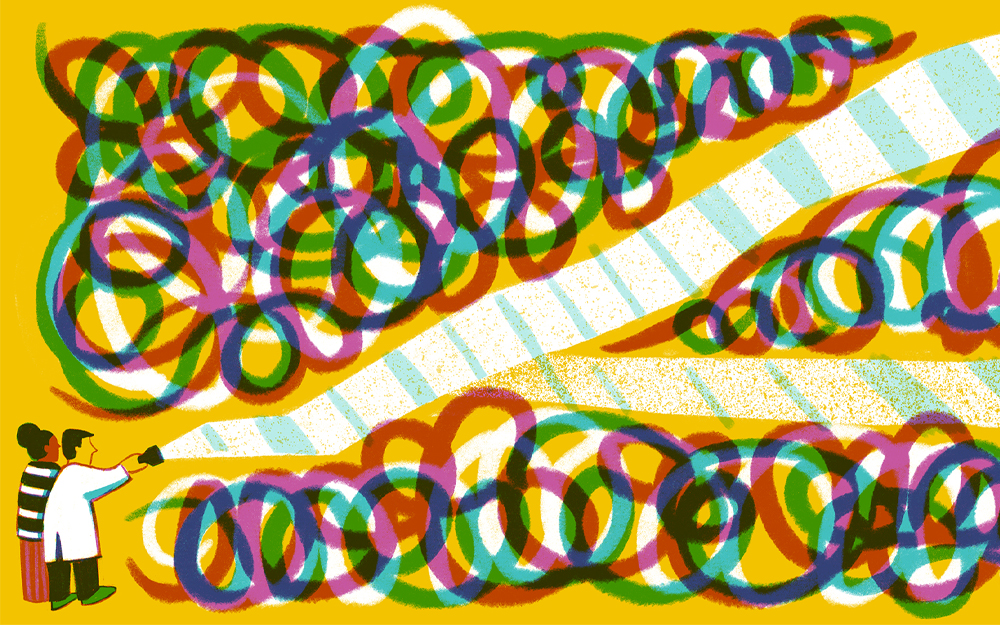
Side by side: Minimally invasive vs. traditional open lung transplant
During a traditional open surgery bilateral lung transplant, the surgeon opens the chest cavity with a clamshell incision, stretching from one armpit across the chest to the other, and breaks the sternum across the middle to access the lungs. The patient is placed on a heart-lung machine during the surgery, which averages six hours.
In contrast, surgeons at the Hannover School in Germany pioneered a minimally invasive lung transplant method, modifying the traditional technique to facilitate a minimally invasive approach. Prior to joining Cedars-Sinai as director of Aortic Surgery, Pedro Catarino, MD, was part of the team pioneering the procedure in England. He later served as director of transplantation at Royal Papworth Hospital in Cambridge, where he taught the procedure to dozens of surgeons, including members of the Smidt Heart Institute transplant team at Cedars-Sinai.
During a minimally invasive bilateral lung transplant, the surgeon accesses the lung via 3-inch (or less) incision under the nipple. The patient's lung is deflated before removal, and the donor's lung is deflated before insertion. Specialized instruments and customized clamps are utilized, as the incision is too small for a surgeon’s hand. A long device is used along with a knot-pusher instrument to aid in the procedure. Orthopaedic dissolvable structures assist in closing the incision.
With less time needed to open and close the patient and control bleeding, the procedure can be performed in 45 minutes to an hour per lung, shortening the time in the OR and eliminating the need for a heart-lung machine during surgery. In contrast to the open approach, where surgeons may be rushed or need to address organs simultaneously while the patient is open, the minimally invasive approach enables the team to isolate focus on a single organ at a time.
Postoperative care

Reinaldo Rampolla, MD, Coburn’s pulmonologist and the medical director of the Lung Transplant Program, assisted in perioperative care. Following the procedure, Rampolla monitored Coburn’s hospital recovery, which lasted nine days compared to the weekslong stays associated with traditional open surgery. “We are already seeing these patients recover much faster with this minimally invasive approach,” Rampolla said.
Following surgery, patients’ new lungs require mechanical ventilation until the body heals from the trauma of surgery and the patient can breathe independently. Traditionally, patients receiving bilateral lung transplants remain intubated and rely on the ventilator until their post-op pain is controlled. With a minimally invasive surgery, the body’s burden to recover is lessened, so patients can be extubated sooner.
“The bottom line is that recovery from minimally invasive lung transplant takes days rather than weeks,” Catarino said. Reducing recovery time produces additional benefits for patients: shorter hospital stays, reduced risk for post-op infection and reduced need for medication, including opioids.
In the year following transplant, patients receive intensive continued care from Cedars-Sinai’s pulmonologists. With specialized lung transplant training, Rampolla and his team are equipped to address the unique medical needs, including immune system suppression, of patients on their path toward health.
The Cedars-Sinai difference
Cedars-Sinai is one of the only medical centers in Southern California with Medicare certification for lung transplants. Patients benefit from the collaborative approach to care that Cedars-Sinai provides. Care teams consisting of surgeons, pulmonologists, diagnostic imaging specialists and specially trained transplant nurses work together to guide patients from procedure to recovery and beyond. The center accepts advanced and challenging cases, and ranked #3 in the nation for pulmonology and lung surgery by U.S. News & World Report.
Across surgical specialties, experts at Cedars-Sinai are world-renowned for their innovative use of minimally invasive approaches. Surgeons perform at the leading edge of minimally invasive procedures in operating suites equipped with the necessary specialized tools and imaging capabilities. Anesthesiologists have extensive expertise in facilitating minimally invasive procedures, and specialized surgical and ICU nursing teams augment the care team.
The future of lung transplant
Catarino recommends minimally invasive approaches as a first option and default operation for most patients requiring a lung transplant. “While more technically challenging for the surgeon, minimally invasive approaches have a greater success rate,” he said. “There is a greater learning curve for this procedure, and Cedars-Sinai has the opportunity to train surgeons all over the world.”
In addition to pioneering transplant techniques, Cedars-Sinai is employing novel procedures to both expand the pool of donor lungs available and ensure healthier donor organs. Traditionally in the United States, transplant surgeons rely almost exclusively on organ donation after brain death (DBD). In Europe and the U.K., organ donation after circulatory death (DCD) supplies up to 40% of transplants. Additionally, Catarino’s research focuses on using machine perfusion to better preserve donor organs. Together, these methods lead to more and healthier donor organs, the key to making lung transplant a viable option for patients.
Who is a good candidate for minimally invasive bilateral lung transplant?
Factoring in Coburn’s critical need for the transplant and enthusiasm for the smaller incision, Catarino considered him an excellent candidate for the minimally invasive approach. Coburn was the first patient to undergo a minimally invasive bilateral lung transplant at Cedars-Sinai.
The majority of transplant patients at Cedars-Sinai are over the age of 70, and the procedure is of particular benefit to older and frailer patient populations. “We have the opportunity for a strong success rate based on the novel surgical option,” Catarino said. The approach is not ideal for patients needing a redo lung transplant.
Getting back on the bike
Coburn is delighted with the results of his surgery—a speedy recovery with minimal cosmetic scarring. “I was so fortunate and felt so proud to be the first. I’m truly lucky,” he said. In the months after his surgery, he is going for daily walks with his wife. As his recovery progresses, he is looking forward to resuming an active lifestyle, including playing tennis and getting back on his bike—shirtless.